Pancreatic Cancer
Pancreatic cancer begins in the tissues of your pancreas — an organ in your abdomen that lies horizontally behind the lower part of your stomach. Your pancreas releases enzymes that aid digestion and hormones that help manage your blood sugar.
Pancreatic cancer typically spreads rapidly to nearby organs. It is seldom detected in its early stages. But for people with pancreatic cysts or a family history of pancreatic cancer, some screening steps might help detect a problem early. One sign of pancreatic cancer is diabetes, especially when it occurs with weight loss, jaundice, or pain in the upper abdomen that spreads to the back.

Pancreatic Cancer Treatment in India may include surgery, chemotherapy, radiation therapy, or a combination of these.
Symptoms of Pancreatic Cancer
- Pain in the upper abdomen that radiates to your back
- Loss of appetite or unintended weight loss
- New-onset diabetes
- Fatigue
- Yellowing of your skin and the whites of your eyes (jaundice)
Factors that may increase your risk of pancreatic cancer include:
- Pancreatitis
- Diabetes
- Family history of pancreatic cancer
- Smoking
- Obesity
- Older age, as most people are diagnosed after age 65
Diagnosis of Pancreatic Cancer
- Imaging includes ultrasound, computerized tomography (CT) scans, magnetic resonance imaging (MRI), and, sometimes, positron emission tomography (PET) scans.
- Endoscopic ultrasound (EUS) uses an ultrasound device to make images of your pancreas from inside your abdomen. The device is passed through a thin, flexible tube (endoscope) down your esophagus and into your stomach to obtain the images.
- A biopsy is a procedure to remove a small sample of tissue for examination under a microscope. Experienced Gastroenterologist may obtain a sample of tissue from the pancreas by inserting a needle through your skin and into your pancreas (fine-needle aspiration). Or he or she may remove a sample during EUS, guiding special tools into the pancreas.
- Blood test.
Pancreatic Cancer Treatment in India
Treatment for pancreatic cancer in India depends on the stage and location of the cancer as well as on your overall health and personal preferences. For most people, the first goal of pancreatic cancer treatment is to eliminate cancer, when possible. When that isn’t an option, the focus may be on improving your quality of life and preventing cancer from growing or causing more harm.
Pancreatic cancer treatment may include surgery, radiation, chemotherapy, or a combination of these. When pancreatic cancer is advanced and these treatments aren’t likely to offer a benefit, pancreatic cancer specialists will offer symptom relief (palliative care) that makes you as comfortable as possible.
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care can be used while undergoing aggressive treatments, such as surgery, chemotherapy, and radiation therapy.
When palliative care is used along with other appropriate pancreatic cancer treatments — even soon after the diagnosis — people with cancer may feel better and live longer.
Colon Cancer
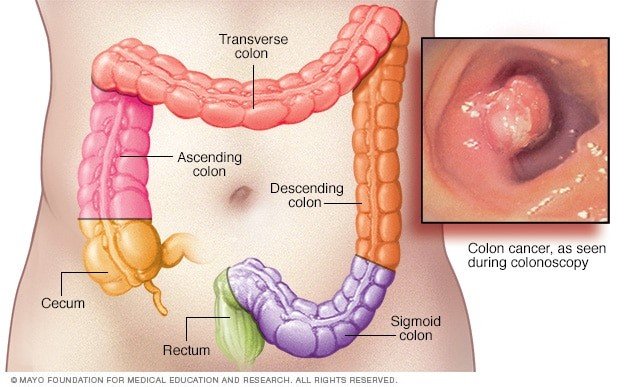
Colon cancer is a type of cancer that begins in the large intestine (colon). The colon is the final part of the digestive tract.
Colon cancer typically affects older adults, though it can happen at any age. It usually begins as small, noncancerous (benign) clumps of cells called polyps that form on the inside of the colon. Over time some of these polyps can become colon cancers.
Polyps may be small and produce few, if any, symptoms. For this reason, doctors recommend regular screening tests to help prevent colon cancer by identifying and removing polyps before they turn into cancer.
If colon cancer develops, many colon cancer treatments are available to help control it, including surgery, radiation therapy, and drug treatments, such as chemotherapy, targeted therapy, and immunotherapy.
Colon cancer is sometimes called colorectal cancer, which is a term that combines colon cancer and rectal cancer, which begins in the rectum.
Signs and symptoms of colon cancer include: persistent change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool, rectal bleeding or blood in your stool, pain, weakness or fatigue, weight loss
In general, colon cancer begins when healthy cells in the colon develop changes (mutations) in their DNA. A cell’s DNA contains a set of instructions that tell a cell what to do.
Healthy cells grow and divide in an orderly way to keep your body functioning normally. But when a cell’s DNA is damaged and becomes cancerous, cells continue to divide — even when new cells aren’t needed. As the cells accumulate, they form a tumor.
With time, the cancer cells can grow to invade and destroy normal tissue nearby. And cancerous cells can travel to other parts of the body to form deposits there (metastasis).
Factors that may increase your risk of colon cancer include:
- Older age. Colon cancer can be diagnosed at any age, but a majority of people with colon cancer are older than 50.
- A personal history of colorectal cancer or polyps.
- Inflammatory intestinal conditions.
- Inherited syndromes that increase colon cancer risk.
- Family history of colon cancer.
- Low-fiber, high-fat diet.
- A sedentary lifestyle.
- Radiation therapy for cancer.
Screening colon cancer
Experienced gastroenterologists recommend that people with an average risk of colon cancer consider colon cancer screening around age 50. However, people with an increased risk, such as those with a family history of colon cancer, should consider screening sooner.
Several screening options exist — each with its benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you.
Screening for colon cancer
Doctors recommend certain screening tests for healthy people with no signs or symptoms to look for signs of colon cancer or noncancerous colon polyps. Finding colon cancer at its earliest stage provides the greatest chance for a cure. Screening has been shown to reduce your risk of dying of colon cancer.
Doctors generally recommend that people with an average risk of colon cancer begin screening around age 50. But people with an increased risk, such as those with a family history of colon cancer should consider screening sooner.
Several screening options exist — each with its benefits and drawbacks. Talk about your options with a Gastroenterologist, and together you can decide which tests are appropriate for you. If a colonoscopy is used for screening, polyps can be removed during the procedure before they turn into cancer.
Diagnosing colon cancer
A colonoscopy uses a long, flexible, and slender tube attached to a video camera and monitor to view your entire colon and rectum. If any suspicious areas are found, your doctor can pass surgical tools through the tube to take tissue samples (biopsies) for analysis and remove polyps.
- Blood tests. No blood test can tell you if you have colon cancer. However, your doctor may test your blood for clues about your overall health, such as kidney and liver function tests.
Gastroenterologists may also test your blood for a chemical sometimes produced by colon cancers (carcinoembryonic antigen, or CEA). Tracked over time, the level of CEA in your blood may help your doctor understand your prognosis and whether your cancer is responding to treatment.
Staging tests may include imaging procedures such as abdominal, pelvic, and chest CT scans. In many cases, the stage of your cancer may not be fully determined until after colon cancer surgery.
Colon Cancer Treatment in India
Treatment for colon cancer in India usually involves surgery to remove the cancer. Other treatments, such as radiation therapy and chemotherapy, might also be recommended.
Your physician will work with you to review your treatment options and choose the best colon cancer treatment that best suits your needs and goals.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care is provided by a team of doctors, nurses, and other specially trained gastroenterologists who work with you, your family, and your other doctors to provide an extra layer of support that complements your ongoing care.